Your mouth is speaking a language most people never learned to understand. Every time you brush your teeth, glance in the mirror, or bite into an apple, your oral tissues are broadcasting signals about what's happening deep inside your body. The question is: are you listening?
Imagine walking into your dental appointment thinking about a simple cleaning, only to have Dr. Malek pause during the examination and say, "I'm noticing some patterns here that suggest we should talk about your overall health." That moment of connection, when oral health becomes a window rather than just a destination, changes everything about how we think about dental care.
The ancient physicians understood something we're only now rediscovering through modern wellness approaches: the mouth is not an isolated system operating independently from the rest of the body. It's an integrated part of your overall health ecosystem, constantly reflecting and influencing what's happening throughout your entire system. When inflammation develops in your gums, when your tongue changes texture or color, when your tooth enamel begins to erode in specific patterns, your body is trying to communicate something important.
This isn't about creating anxiety or transforming every dental visit into a diagnostic mystery. Instead, it's about recognizing the profound opportunity that exists when we pay attention to oral health as a meaningful indicator of overall wellness. Your mouth can serve as an early warning system, a preventive health tool, and a gateway to understanding your body's needs before small concerns become significant challenges.
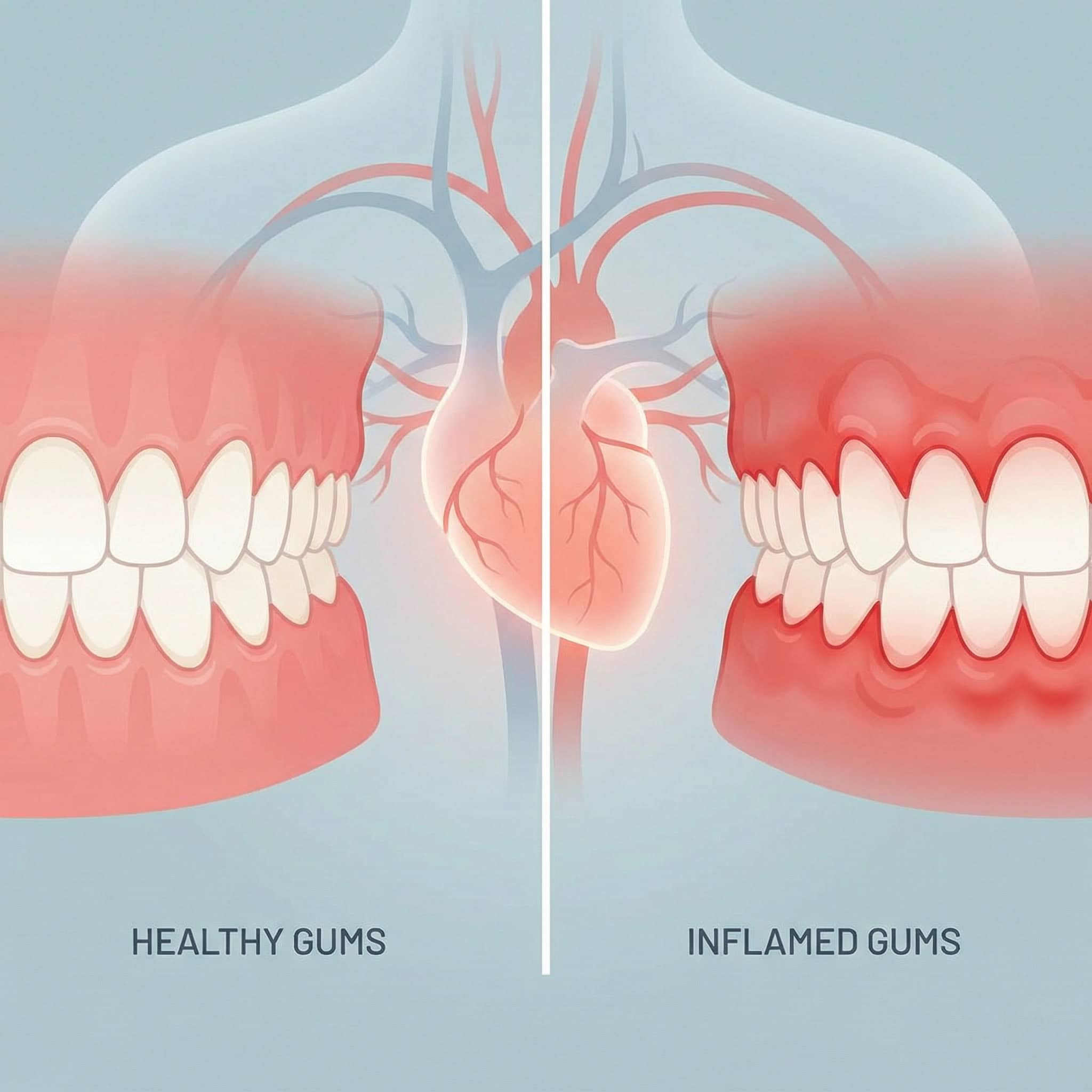
The Inflammation Connection: When Your Gums Tell Your Heart's Story
Picture inflammation as a conversation your body is having with itself, a continuous dialogue about threats, healing, and balance. When that conversation becomes chronic and unresolved, it doesn't stay localized. The inflammatory response that begins in your gum tissue doesn't recognize boundaries or borders within your body. It sends signals, triggers responses, and creates patterns that ripple through your cardiovascular system.
The tissue in your gums is remarkably similar to the tissue lining your blood vessels. Both are designed to serve as protective barriers, both respond to bacterial presence, and both participate in your body's inflammatory response system. When gum tissue becomes chronically inflamed, swollen, and prone to bleeding, it's demonstrating an inflammatory pattern that often mirrors what's happening in blood vessel walls throughout your body.
Consider how this connection manifests in everyday experience. The same lifestyle factors that contribute to gum inflammation—stress, poor nutrition, inadequate sleep, smoking—are also known contributors to cardiovascular concerns. The bacteria that colonize inflamed gum pockets don't stay confined to your mouth. They enter your bloodstream through the tiny wounds that develop in diseased gum tissue, traveling throughout your circulatory system and potentially contributing to inflammation far from their point of origin.
This bidirectional relationship means that addressing oral inflammation isn't just about saving your teeth or freshening your breath. It's about reducing overall systemic inflammation and supporting your cardiovascular system's ability to function optimally. When Dr. Malek measures pocket depths around your teeth and assesses gum tissue health, they're gathering information that has implications far beyond your smile.
The empowering aspect of this connection is that it works in both directions. Improving your oral health through consistent home care, professional cleanings, and addressing active gum disease can contribute to reducing overall inflammatory burden on your body. Every time you floss, you're not just preventing cavities; you're potentially supporting your heart health. Every professional cleaning that removes calculus and reduces bacterial load is an investment in your overall wellness, not just your dental health.
Your Mouth as a Nutritional Report Card
The tissues inside your mouth are among the fastest-growing cells in your body, constantly regenerating and renewing themselves. This rapid turnover makes them exquisitely sensitive to nutritional status. When your body lacks specific nutrients or struggles to absorb what you're providing, your oral tissues often show the signs before other, slower-growing tissues reveal the deficiency.
Think about the last time you accidentally bit your cheek or burned your tongue on hot coffee. Within days, that injury had healed, often without you consciously noticing the repair process. This remarkable healing capacity depends on adequate nutrition—not just calories, but the specific building blocks your body needs to construct healthy tissue. When those building blocks are missing or insufficient, the healing slows, the tissue quality diminishes, and visible changes begin to appear.
Your tongue serves as a particularly revealing canvas for nutritional status. Changes in color, texture, and surface appearance can reflect deficiencies in iron, B vitamins, and other essential nutrients. A persistently pale tongue might suggest inadequate iron levels, while a smooth, glossy appearance could indicate B vitamin deficiencies. These aren't diagnostic certainties, but they are meaningful signals that warrant attention and possibly further investigation.
The health and integrity of your gum tissue also depends heavily on nutritional status, particularly vitamin C and other antioxidants that support collagen production and tissue repair. When nutrition is inadequate, gums may appear pale rather than healthy pink, heal slowly after injury, and become more susceptible to inflammation and infection. The connection between scurvy and gum disease in historical contexts demonstrates this relationship in its most extreme form, but subtler nutritional insufficiencies create subtler but still significant effects.
Even your saliva composition and production levels reflect nutritional and hydration status. Adequate saliva flow depends on proper hydration and certain nutrients, and saliva itself contains proteins, minerals, and enzymes that your body constructs from the raw materials you provide through diet. When you experience persistent dry mouth unrelated to medications or medical conditions, it might be your body's way of signaling that it lacks the resources to maintain optimal saliva production.
This nutritional connection transforms how we think about oral health maintenance. Yes, brushing and flossing remove bacteria and prevent decay. But supporting your oral health also means nourishing your body with the building blocks it needs to maintain resilient tissue, produce protective saliva, and heal efficiently from the minor injuries that occur daily. Your dental health becomes an invitation to consider whether you're truly nourishing yourself at a cellular level.
The Practical Reality of Nutritional Support
Understanding these connections doesn't require becoming obsessed with every vitamin and mineral. Instead, it invites a broader perspective on oral health that includes asking questions about overall nourishment. Are you eating a variety of whole foods that provide diverse nutrients? Are you staying adequately hydrated throughout the day? Are you supporting your body's ability to absorb and utilize the nutrients you consume?
When you notice changes in your oral tissues—increased sensitivity, slower healing, changes in appearance—these observations become data points that might prompt you to consider your overall nutritional approach. Rather than viewing these signs with alarm, you can see them as valuable feedback from a body that's constantly trying to communicate its needs.
The Digestive Connection: When Tooth Enamel Tells a Stomach Story
Your tooth enamel is the hardest substance in your body, designed to withstand years of chewing, temperature changes, and exposure to various foods and beverages. Yet this remarkable material has a vulnerability: acid. When the pH in your mouth drops below a certain threshold, enamel begins to dissolve, losing minerals in a process called demineralization. While some acid exposure is normal and manageable, chronic acid exposure creates distinctive erosion patterns that tell a story about what's happening in your digestive system.
The erosion pattern matters because it reveals the source of the acid. Dietary acids from frequent consumption of acidic foods and beverages create one pattern, typically affecting the front surfaces of teeth. But erosion on the tongue side of teeth, particularly the back teeth, often suggests acid coming from within the digestive system rather than from external dietary sources.
Imagine your digestive system as a carefully controlled environment where acid belongs in specific places and is buffered and managed through various mechanisms. When that control breaks down—when acid frequently moves upward from the stomach into the esophagus and sometimes into the mouth—it creates opportunities for that acid to contact tooth enamel from the inside out. This might happen during obvious reflux episodes, but it can also occur silently during sleep or in subtle ways that you might not consciously notice.
The connection extends beyond just acid exposure. The bacterial balance in your mouth is part of a larger microbiome that extends throughout your digestive system. Disruptions in gut bacterial balance can influence oral bacterial populations, potentially affecting both decay risk and gum health. The relationship between oral health and digestive function flows in both directions, with each system influencing the other through shared bacterial populations, immune responses, and inflammatory patterns.
For people struggling with digestive concerns, paying attention to oral health becomes another tool for understanding and managing their overall wellness. Changes in tooth sensitivity, increases in decay despite good oral hygiene, or specific erosion patterns might prompt important conversations with healthcare providers about digestive function and the potential need for intervention.
This connection also highlights why comprehensive dental examinations involve more than just looking at teeth and gums. At The Harmony Dental Group, Dr. Malek and the team take time to understand erosion patterns, ask questions about digestive symptoms, and consider the whole person rather than just the mouth, identifying concerns that might benefit from multidisciplinary attention. Your dental visit becomes an opportunity for collaborative health assessment rather than isolated dental evaluation.
The Oral Microbiome: Your Mouth's Microscopic Ecosystem
Right now, hundreds of bacterial species are living in your mouth, forming complex communities on your teeth, tongue, and soft tissues. Before you feel alarmed, understand that this is not only normal but essential. Your oral microbiome, like the more widely discussed gut microbiome, is a sophisticated ecosystem where bacterial balance determines health outcomes more than bacterial presence itself.
Think of your oral microbiome as a garden. In a healthy garden, diverse plants coexist in balance, with beneficial species thriving and keeping problematic species in check through competition for resources and space. When the garden becomes imbalanced—perhaps through poor soil quality, inadequate water, or disruption of beneficial species—opportunistic weeds can take over and dominate the landscape. Your mouth works similarly, with beneficial bacterial species helping maintain balance and prevent harmful species from establishing dominance.
This ecosystem doesn't exist in isolation from the rest of your body. The bacteria in your mouth are in constant communication with your immune system, training it, challenging it, and influencing how it responds to threats throughout your body. Some oral bacteria produce compounds that enter your bloodstream and influence inflammation levels systemically. Others interact with immune cells in ways that can either support or compromise immune function depending on the balance and health of the overall community.
The relationship between your oral microbiome and overall wellness extends to unexpected areas. Emerging understanding suggests connections between oral bacterial populations and everything from immune function to metabolic health. The mechanisms are complex and still being understood, but the basic principle is clear: the microscopic ecosystem in your mouth participates in your body's larger health conversations in ways we're only beginning to appreciate.
What influences the health and balance of this ecosystem? Many of the same factors that influence gut microbiome health: diet, stress levels, medication use, sleep quality, and overall immune function. Excessive sugar provides fuel for decay-causing bacteria, allowing them to outcompete more beneficial species. Chronic stress can alter saliva composition and pH, creating environmental conditions that favor problematic bacterial populations. Antibiotics, while sometimes necessary, can disrupt bacterial balance both in the gut and the mouth, sometimes requiring intentional efforts to support healthy recolonization.
Supporting Your Oral Ecosystem
Understanding the oral microbiome as an ecosystem rather than an enemy to be eradicated changes how we approach oral health maintenance. The goal isn't sterility or the elimination of all bacteria—that's neither possible nor desirable. Instead, the goal is supporting conditions that allow beneficial species to thrive while keeping potentially problematic species in check.
This means consistent mechanical cleaning to disrupt bacterial films before they mature into problematic communities. It means managing dietary sugar to avoid providing excessive fuel for decay-causing species. It means maintaining good saliva flow through adequate hydration and addressing dry mouth conditions. And it means recognizing that your oral microbiome health is connected to your overall wellness, influenced by factors like stress, sleep, nutrition, and immune function that extend far beyond brushing and flossing.
The Stress-Inflammation-Oral Health Triangle
Your body responds to stress through ancient mechanisms designed for short-term threats—the famous fight-or-flight response that redirects resources to immediate survival. But when stress becomes chronic, when those emergency response systems never fully turn off, the effects ripple through every system in your body, including your mouth.
Chronic stress influences oral health through multiple interconnected pathways. It affects your immune system's ability to manage the bacterial populations in your mouth, potentially allowing opportunistic species to flourish. It can alter saliva composition and flow, reducing your mouth's natural protective mechanisms. It often leads to unconscious behaviors like teeth grinding or clenching, creating physical stress on teeth, jaw joints, and surrounding structures. And it contributes to systemic inflammation, which amplifies inflammatory responses in gum tissue and throughout your body.
Consider how this manifests in real experience. During particularly stressful periods, you might notice your gums becoming more sensitive or prone to bleeding, even if your oral hygiene habits haven't changed. You might wake with jaw soreness or tension headaches from nighttime clenching you're not consciously aware of. You might experience more frequent canker sores or other oral tissue irritations. These aren't coincidental occurrences—they're your body demonstrating the integrated nature of stress, immune function, and oral health.
The relationship works in multiple directions. Chronic oral pain or dental anxiety can contribute to overall stress burden, creating a cycle where stress affects oral health, and oral health concerns generate more stress. Breaking this cycle often requires addressing both the physical oral health concerns and the stress patterns that contribute to and result from those concerns.
Sleep quality enters this triangle as well, since stress often disrupts sleep, and poor sleep intensifies stress responses and inflammatory patterns. The grinding and clenching that often accompany stress frequently intensify during sleep, when conscious control is absent. Poor sleep also impairs immune function, potentially affecting your body's ability to maintain healthy bacterial balance in your mouth and manage gum tissue inflammation.
Understanding these connections transforms oral health care from a purely mechanical maintenance task into a holistic wellness practice. When you notice increased oral health concerns during stressful periods, you're observing real physiological connections, not imagining problems. Your body is demonstrating through your oral health that stress management isn't a luxury or an indulgence—it's a fundamental component of physical health maintenance.
The Integration Point
This stress-inflammation-oral health triangle reveals why comprehensive dental care must consider the whole person, not just the teeth and gums. Questions about stress levels, sleep quality, and stress management strategies become relevant to oral health assessment. Recommendations might extend beyond brushing and flossing to include stress reduction approaches, sleep hygiene improvements, or even referrals to other healthcare providers who can address the broader wellness picture.
For you as a patient, this integration means recognizing that taking care of your oral health sometimes means taking care of your stress levels, your sleep quality, and your overall inflammatory burden. The mouth becomes a feedback system that can help you recognize when stress is affecting your physical health in measurable ways, prompting you to prioritize stress management not as self-indulgence but as health maintenance.
Transforming Your Next Dental Visit
Armed with this understanding of how your oral health reflects and influences your overall wellness, your next dental appointment transforms from a routine cleaning into a comprehensive health screening opportunity. The examination becomes a chance to gather valuable information about inflammation levels, nutritional status, stress impacts, digestive health patterns, and microbiome balance—all through careful attention to the signals your mouth is broadcasting.
This doesn't mean Dr. Malek will diagnose digestive disorders, prescribe stress management programs, or make definitive pronouncements about your heart health. But it does mean that careful observation of oral health patterns can identify areas worth discussing, concerns worth monitoring, and opportunities for preventive intervention before small issues become significant problems.
The shift in perspective this creates is profound. Dental care moves from reactive treatment of problems to proactive wellness monitoring. Your six-month cleaning becomes an opportunity to check in on how your whole body is functioning, using your mouth as a remarkably revealing window into overall health status. The time invested in comprehensive dental care becomes time invested in total body wellness, with potential benefits extending far beyond preventing cavities and gum disease.
This integrated approach to oral health also changes how you think about daily oral hygiene practices. Brushing and flossing aren't just mechanical tasks to prevent tooth decay—they're wellness practices that support your immune system, reduce inflammatory burden, maintain healthy bacterial balance, and contribute to overall health maintenance. The two minutes twice daily you spend on oral hygiene becomes a meaningful investment in your total wellness, not just your smile.
Consider what this means for preventive health strategy. While you might hesitate to schedule medical appointments without specific symptoms prompting concern, regular dental visits already provide built-in opportunities for comprehensive health screening. Taking full advantage of these appointments means being open about overall health concerns, asking questions about what your oral health might be revealing, and partnering with Dr. Malek and The Harmony Dental Group to understand the bigger picture your mouth is painting about your wellness.
Your Mouth Is Speaking—Are You Ready to Listen?
The mouth you see in the mirror each morning is doing far more than chewing food and forming words. It's serving as a continuous health monitoring system, broadcasting signals about inflammation, nutrition, stress, digestive function, and immune status. These signals are always present, always available, if you know how to interpret them and take the time to pay attention.
This isn't about becoming hypervigilant or anxious about every minor oral health variation. It's about recognizing the profound integration between oral health and overall wellness, using that knowledge to inform more comprehensive self-care, and partnering with Dr. Malek and the team at The Harmony Dental Group who understand and embrace this holistic perspective.
Your next dental appointment is an opportunity to begin this integrated approach to wellness. Come prepared to discuss not just your teeth and gums, but your overall health patterns, concerns, and questions. Be open to the possibility that oral health observations might prompt broader wellness conversations. View the comprehensive examination as exactly that—a thorough assessment of what your oral health reveals about your overall wellbeing.
The mouth speaks a language of health and wellness. Learning to understand that language, and partnering with Dr. Malek and The Harmony Dental Group, who understand it fluently, transforms dental care from isolated maintenance into integrated wellness practice. Your smile isn't just about appearance—it's a window into your body's inner workings, a tool for early detection of concerns, and an opportunity for preventive health intervention.
What is your mouth trying to tell you about your health? There's only one way to find out: schedule a comprehensive examination with Dr. Malek and The Harmony Dental Group, who understand that oral health and overall health are inseparably connected. Your body is constantly communicating through your oral tissues. Isn't it time you started listening?
Discover What Your Smile Reveals About Your Health
At The Harmony Dental Group, we believe comprehensive dental care means understanding the whole person, not just the teeth and gums. Our thorough examinations go beyond surface-level cleaning to assess what your oral health might be revealing about your overall wellness. Schedule your wellness-focused dental visit today and discover the insights your mouth has been trying to share.
Ready to transform your approach to oral health? Contact The Harmony Dental Group's Norwalk office to schedule your comprehensive examination and begin your journey toward integrated wellness through exceptional dental care.
Frequently Asked Questions
1. How can I tell if my oral health is affecting my overall health?
Changes in your oral health can manifest in various ways, such as increased sensitivity, bleeding gums, or persistent bad breath. These symptoms may indicate underlying issues like inflammation or nutritional deficiencies that could impact your overall health. Regular dental check-ups can help identify these signs early. Additionally, being aware of your body's signals, such as changes in your mouth's appearance or function, can provide valuable insights into your overall wellness. If you notice any concerning changes, consult Dr. Malek at The Harmony Dental Group for a comprehensive evaluation.
2. What role does nutrition play in maintaining oral health?
Nutrition is crucial for maintaining healthy oral tissues and preventing diseases. Essential nutrients like vitamins C and D, calcium, and B vitamins support gum health, tissue repair, and enamel strength. A balanced diet rich in whole foods can help your body regenerate oral tissues effectively. Conversely, deficiencies can lead to issues like gum disease or slow healing. Staying hydrated is also vital, as it supports saliva production, which protects against decay and maintains oral health. Consider your diet as a foundational aspect of your oral care routine.
3. How does stress impact my oral health?
Chronic stress can significantly affect your oral health by altering your immune response, leading to increased susceptibility to gum disease and other oral issues. Stress may also cause behaviors like teeth grinding or jaw clenching, which can result in tooth wear and jaw pain. Additionally, stress can reduce saliva production, diminishing your mouth's natural defenses against bacteria. Managing stress through relaxation techniques, exercise, and adequate sleep can help mitigate these effects and promote better oral health.
4. What should I discuss with my dentist during my next visit?
During your next dental appointment, consider discussing any changes you've noticed in your oral health, such as sensitivity, bleeding, or unusual lesions. It's also beneficial to talk about your overall health, including stress levels, dietary habits, and any medications you are taking. This information can help Dr. Malek assess your oral health in the context of your overall wellness. Don't hesitate to ask questions about how your oral health might reflect other health issues, as this can lead to a more comprehensive care plan.
5. Can oral health affect my cardiovascular health?
Yes, there is a significant connection between oral health and cardiovascular health. Chronic gum disease can lead to systemic inflammation, which may contribute to heart disease. The bacteria from inflamed gums can enter the bloodstream, potentially affecting blood vessels and heart function. Maintaining good oral hygiene through regular brushing, flossing, and dental visits can help reduce the risk of gum disease and, consequently, support cardiovascular health. It's essential to view oral care as part of your overall health strategy.
6. How can I improve my oral microbiome health?
To enhance your oral microbiome health, focus on maintaining a balanced diet low in sugar and high in fiber, which supports beneficial bacteria. Regular brushing and flossing help disrupt harmful bacterial growth, while staying hydrated promotes saliva production, which is crucial for a healthy oral environment. Additionally, consider incorporating probiotics into your diet, as they can help restore balance to your oral microbiome. Avoiding excessive antibiotic use, unless necessary, is also important, as antibiotics can disrupt the natural bacterial balance in your mouth.
7. What are the signs of nutritional deficiencies reflected in oral health?
Signs of nutritional deficiencies can often be observed in your oral health. For instance, a pale tongue may indicate iron deficiency, while a smooth, glossy appearance could suggest a lack of B vitamins. Gums that heal slowly or appear pale may signal inadequate vitamin C intake. Additionally, persistent dry mouth can indicate dehydration or insufficient nutrient intake. If you notice these changes, it may be beneficial to consult with a healthcare provider to assess your nutritional status and make necessary dietary adjustments.
About The Harmony Dental Group
The Harmony Dental Group, led by Dr. Malek, is dedicated to providing comprehensive dental care that integrates oral health with overall wellness. Our practice emphasizes a holistic approach, recognizing the profound connections between your mouth and the rest of your body. We are committed to empowering our patients with knowledge and personalized care plans that extend beyond traditional dentistry, fostering long-term health and well-being.