Understanding Dental Implants: Your Comprehensive Resource for Smile Restoration
Dental implants offer a life-changing solution for those struggling with missing teeth. This comprehensive guide will explore the types of dental implants available, the step-by-step procedure, and who makes an ideal candidate. Readers will gain valuable insights into the cost of dental implants and learn essential maintenance tips for long-lasting results. By the end of this article, you'll have the knowledge needed to make an informed decision about restoring your smile with dental implants.
Key Takeaways
- Dental implants provide a durable, long-lasting solution for replacing missing teeth and preserving oral health
- The implant procedure involves surgical placement, healing, and restoration stages, typically spanning several months
- Proper oral hygiene and regular dental check-ups are essential for maintaining dental implant health
- Implant costs vary but may offer long-term value compared to alternatives like bridges or dentures
- Early detection and treatment of implant issues can significantly improve outcomes and longevity
Understanding Dental Implants and Their Purpose
Dental implants offer a durable solution for replacing missing teeth, restoring both function and appearance. These artificial tooth roots, endorsed by the American Academy of Dental Implantology, provide stability and prevent bone loss. Unlike traditional dentures, implants distribute pressure evenly, preserving surrounding tissue. Patients seeking to find a doctor for implant treatment can expect long-lasting results and improved oral health.
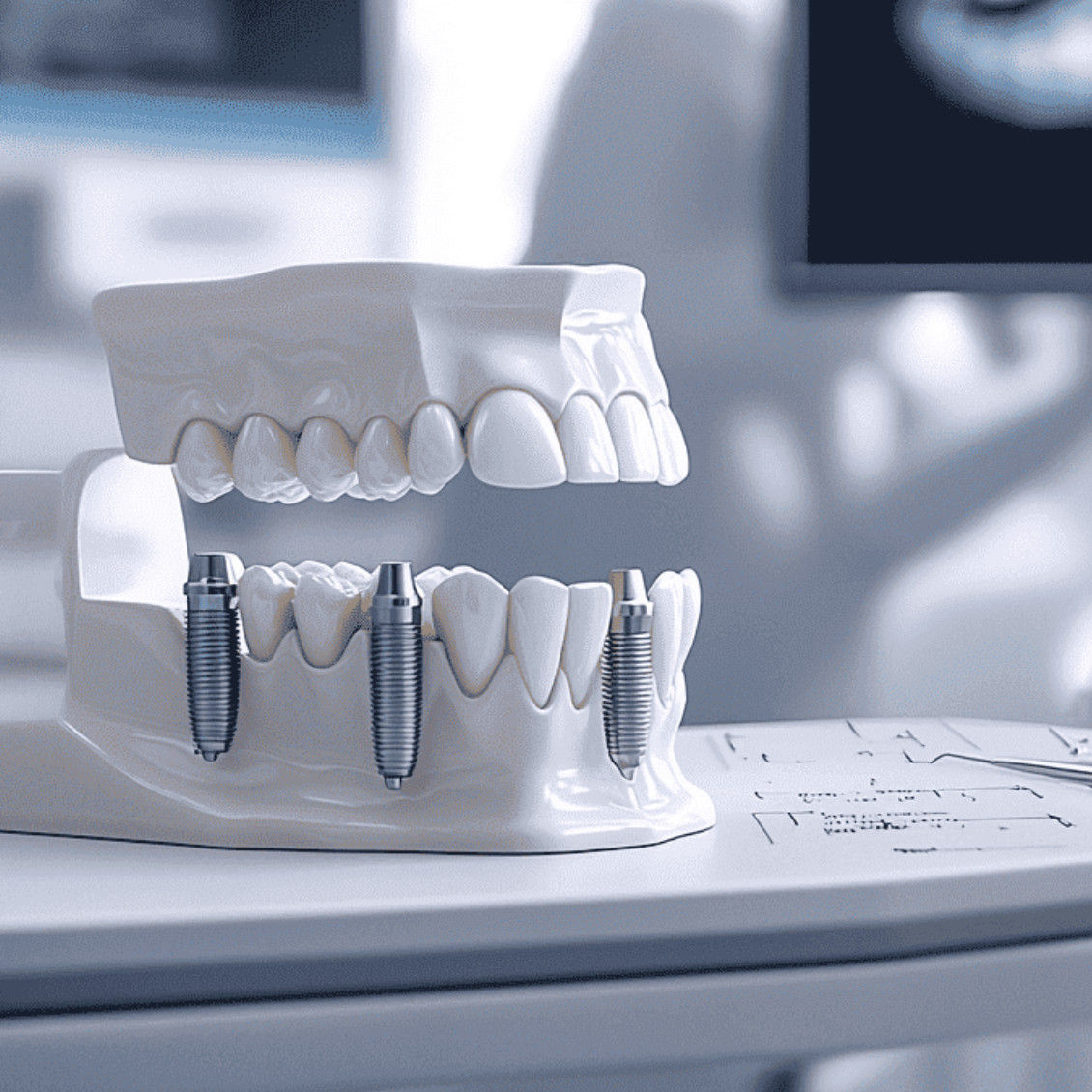
Definition and Function of Dental Implants
Dental implants are artificial tooth roots surgically placed into the dental arch to support replacement teeth. These titanium posts fuse with the jawbone, creating a stable foundation for crowns that restore function and aesthetics. The implant integrates with the surrounding nerve tissue, providing a natural feel and sensation.
The primary function of dental implants is to replace missing teeth and prevent bone loss in the jaw. They distribute chewing forces evenly across the dental arch, preserving adjacent teeth and maintaining facial structure. Patients undergoing implant surgery may receive nitrous oxide for comfort.
Benefits of Choosing Dental Implants for Smile Restoration
Dental implants offer significant benefits for smile restoration, promoting overall oral health and preserving bone structure. These permanent solutions provide a stable foundation for chewing, preventing further tooth loss and maintaining facial aesthetics. In cases where bone density is insufficient, a bone graft procedure can prepare the jaw for successful implant placement.
The All-on implant technique, known as "Allon," revolutionizes full-arch restoration by supporting an entire set of teeth with just four to six strategically placed implants. This approach maximizes the use of available bone, often eliminating the need for extensive grafting procedures. Patients experience improved chewing function and confidence in their restored smiles, contributing to better overall health and quality of life.
Difference Between Dental Implants and Other Tooth Replacement Options
Dental implants stand out from other tooth replacement options due to their unique integration with the jawbone. Unlike traditional dentures or bridges, implants fuse with the hard tissue, creating a stable foundation for the prosthesis. This integration reduces the risk of bone loss and provides a more natural feel when speaking or chewing.
The durability of dental implants, often made from biocompatible alloys, surpasses that of other options. While bridges and dentures may require replacement every 5-10 years, implants can last a lifetime with proper care. Patients find implants easier to maintain, as they can brush and floss normally, unlike the special cleaning routines needed for removable prostheses.
Types of Dental Implants

Dental implants offer various options for smile restoration, including endosteal, subperiosteal, and zygomatic implants. Each type addresses specific patient needs, from standard tooth replacement to complex maxillary sinus cases. Understanding these options helps patients choose the most suitable therapy, reducing the risk of implant failure and ensuring successful outcomes, even in challenging situations like those requiring AllOn treatment.
Endosteal Implants
Endosteal implants stand as the most common type of dental implant, offering a robust solution for tooth loss. These implants, typically made of titanium, are surgically placed directly into the jawbone, providing a stable foundation for artificial teeth. Patients with good oral hygiene can expect long-term success with endosteal implants, as they integrate well with the bone structure.
In cases where insufficient bone density exists, a sinus lift procedure may be necessary before placing endosteal implants. This technique enhances the upper jaw's bone volume, ensuring proper support for the implant. Dentists advise patients with xerostomia to maintain meticulous oral care, as dry mouth can affect implant longevity. Regular check-ups and proper cleaning of the implant site are crucial for preventing complications and ensuring optimal oral health.
Subperiosteal Implants
Subperiosteal implants offer an alternative solution for patients with insufficient jawbone density, as recognized by the American Academy of Periodontology. These implants rest on top of the bone but under the gum, utilizing a metal framework that attaches to the zygomatic bone for support. The procedure requires less extensive osseointegration compared to traditional implants, making it suitable for patients who may not qualify for endosteal implants.
The placement of subperiosteal implants typically involves local anesthesia and a two-stage process. During the first stage, an impression of the jawbone is taken to create a custom-fitted framework. In the second stage, the framework is surgically placed and the gum tissue is allowed to heal around it. This technique provides valuable information for dentists treating patients with compromised bone structure, offering a reliable tooth replacement option when bone grafting is not feasible.
Zygomatic Implants
Zygomatic implants offer a solution for patients with severe maxillary bone loss who may not be candidates for traditional dental implants. These specialized implants anchor into the zygomatic bone, providing support for full-arch restorations even when the maxilla lacks sufficient bone volume. Patients interested in this advanced technique can contact dental offices specializing in zygomatic implants to discuss their options.
Research has shown that zygomatic implants have high success rates and can significantly improve quality of life for patients with complex dental needs. Dental professionals often feature information about zygomatic implants on their websites, allowing potential patients to learn about this innovative treatment. By offering an alternative to extensive bone grafting procedures, zygomatic implants can reduce treatment time and provide a stable foundation for prosthetic teeth.
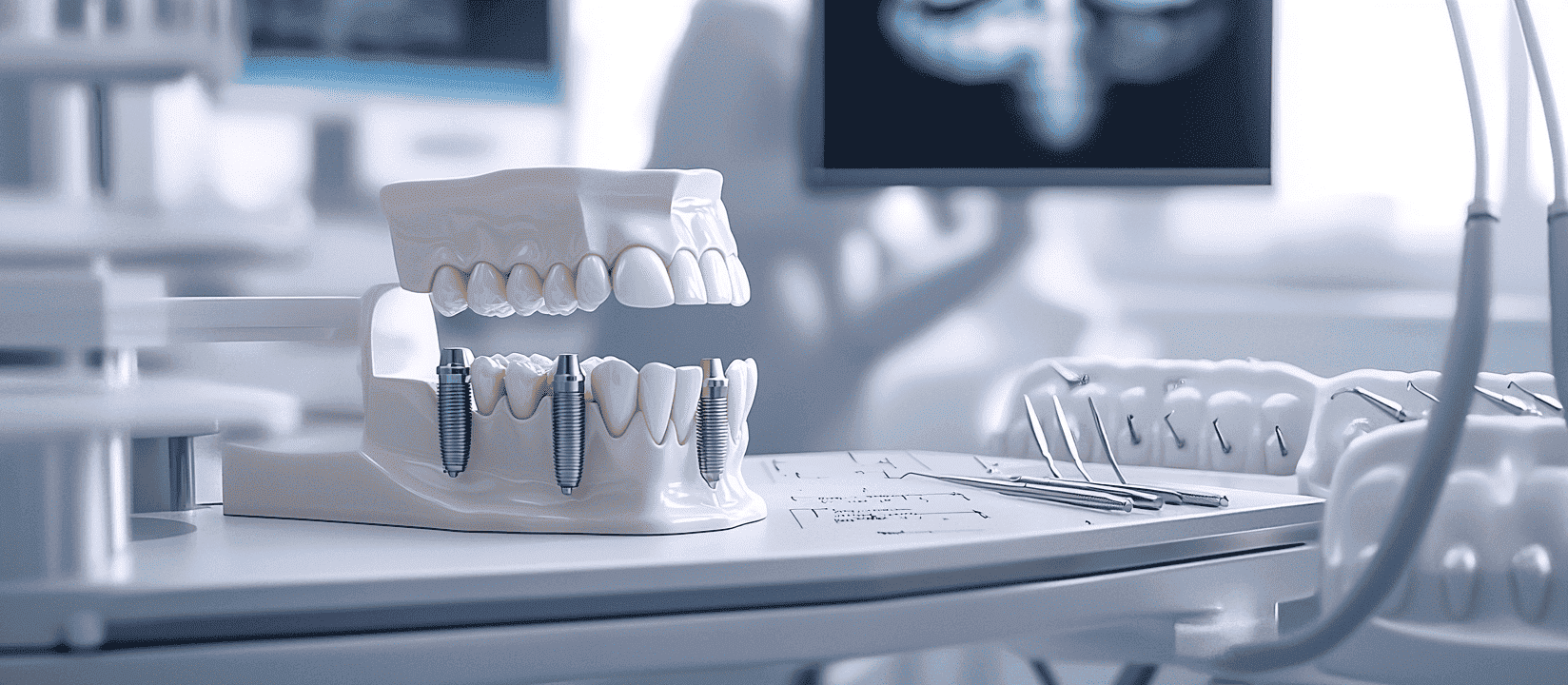
The Dental Implant Procedure
The dental implant procedure involves several stages, from initial consultation to post-surgery care. Patients undergo a thorough assessment before the step-by-step surgical process begins. Various anesthesia and pain management options ensure comfort during the procedure. Proper post-surgery care, including medication and managing potential bleeding, is crucial for successful healing and preventing complications like tooth decay or overdenture issues.
Initial Consultation and Assessment
The initial consultation for dental implants involves a comprehensive assessment of the patient's oral health and medical history. Dentists evaluate factors such as bone density, gum health, and the presence of any medical conditions that may affect healing, including the use of bisphosphonates. This thorough examination helps determine the patient's suitability for dental implants and identifies any potential complications.
During the assessment, dentists may use advanced imaging techniques to visualize the jawbone structure and plan the implant placement. They discuss the procedure in detail, including the use of drills for implant insertion and potential risks such as blood loss. Patients are encouraged to ask questions about mis dent (minimally invasive dentistry) options and how dental implants compare to alternative treatments.
Step-by-Step Surgical Process
The dental implant surgical process begins with the administration of local anesthesia to ensure patient comfort. The dentist creates a small incision in the gum tissue to expose the jawbone, where a precise hole is drilled to accommodate the implant. Patients with allergies to certain materials should inform their dentist beforehand to prevent complications.
Once the implant is placed, the gum tissue is sutured closed, and the healing process begins. During this time, patients may experience temporary bad breath due to bacteria accumulation. The American Academy of Periodontology recommends maintaining excellent oral hygiene to prevent periodontal disease and ensure successful implant integration. The healing period typically lasts several months, allowing the implant to fuse with the bone:
Anesthesia and Pain Management Options
Dental implant procedures typically employ local anesthesia to ensure patient comfort during the surgery. For patients who experience anxiety or require more extensive work, dental public health professionals may recommend sedation options. These can range from nitrous oxide to intravenous sedation, allowing even those who smoke to undergo the procedure comfortably.
Post-operative pain management is crucial for successful dental implant recovery. Dentists often prescribe pain medications and provide instructions for managing discomfort as the replacement tooth integrates with the jawbone. Patients with existing dental work, such as a bridge, may require special considerations to ensure the implant can properly anchor and function alongside other restorations.
Post-Surgery Care
After dental implant surgery, patients must follow strict oral care routines to ensure proper healing and integration of the replacement teeth. The dentist provides detailed instructions on cleaning techniques, including the use of special brushes and rinses to prevent infection around the surgical site. Patients should avoid touching the area with their tongue or fingers to reduce the risk of complications.
In the days following surgery, patients may experience some discomfort in the ear and jaw areas. The dentist typically prescribes pain medication and recommends cold compresses to manage swelling. It's crucial for patients to attend all follow-up appointments to monitor the healing process and address any concerns promptly, ensuring the long-term success of their dental implant procedure.
Who Is a Suitable Candidate for Dental Implants?

Determining dental implant candidacy involves assessing various factors. Patients' oral health, age, and lifestyle habits play crucial roles in eligibility. Proper oral hygiene and healthy gum tissue are essential for successful implant placement. The shape of the jaw and lip position may influence the implant process. Dental professionals consider these aspects to ensure optimal outcomes for patients seeking smile restoration through implants.
Factors Influencing Eligibility for Dental Implants
Dental implant eligibility depends on several factors that dentists assess during the initial consultation. Patients must have adequate bone density in the jaw to support the implant screw, as well as healthy gum tissue free from periodontal disease. Those with certain medical conditions, such as uncontrolled diabetes or a history of radiation therapy to the jaw area, may face increased risks, including osteonecrosis of the jaw.
Dental insurance coverage can influence a patient's decision to pursue dental implants. While many insurance plans do not fully cover implants, some may offer partial benefits. Patients should discuss financing options with their dental provider to explore ways to make this restorative treatment more accessible. The long-term success of dental implants relies on proper oral hygiene and regular dental check-ups:
- Adequate bone density and volume
- Healthy gum tissue
- Commitment to oral hygiene
- Absence of certain medical conditions
- Financial considerations and insurance coverage
Age and Oral Health Considerations
Age does not significantly limit dental implant candidacy, as the jaw and mandible continue to support tooth replacement throughout adulthood. However, younger patients must have completed facial growth before implant placement to ensure proper alignment and function. Dentists assess bone density and overall oral health, including the presence of calculus, to determine suitability for implant surgery.
Proper oral hygiene, including regular use of a toothbrush and professional cleanings, plays a crucial role in implant success. Patients with existing metal restorations may require additional evaluation to ensure compatibility with implant materials. The dentist will consider factors such as gum health, bone quality, and the patient's ability to maintain good oral care when recommending implant treatment.
Lifestyle Factors and Dental Habits
Lifestyle habits significantly impact dental implant candidacy. Patients who smoke or consume excessive alcohol may experience slower healing and increased risk of implant failure. Regular oral hygiene practices, including proper brushing and flossing techniques, are essential for maintaining healthy gums and supporting the long-term success of titanium implants and crowns.
Orthodontics history can affect implant placement, as previous treatments may have altered the position of surrounding teeth. Patients with a history of teeth grinding or clenching may require additional protective measures to safeguard their implants. Dentists assess these factors to determine the most suitable treatment plan, ensuring optimal outcomes for each patient's unique oral health situation.
Cost of Dental Implants

The cost of dental implants varies based on factors such as the number of implants needed and materials used, like titanium alloys. This section breaks down expenses, explores insurance coverage and financing options, and compares long-term costs with alternatives like dentures. Understanding these aspects helps patients make informed decisions about their dental restoration journey.
Breakdown of Expenses Associated With Dental Implants
Dental implant procedures involve several components that contribute to the overall cost. The expense typically includes the surgical placement of the implant, the abutment, and the final crown. Patients should also consider potential additional costs such as sedation, pre-implant procedures like bone grafting, and follow-up appointments to monitor oral health.
Insurance coverage for dental implants varies widely, with some plans offering partial benefits while others may not cover the procedure at all. Patients often need to explore financing options or dental savings plans to manage the investment in their oral health. The cost breakdown for a single dental implant often includes:
Insurance Coverage and Financing Options
Insurance coverage for dental implants varies among providers, with some plans offering partial benefits for prosthodontics procedures. Patients should consult their insurance company to understand their specific coverage for tooth replacement options. Many dental offices offer in-house financing or partner with third-party lenders to make implant treatments more accessible.
For those without insurance or seeking additional financial assistance, dental savings plans and health savings accounts (HSAs) can help offset the cost of implant procedures. These options allow patients to allocate pre-tax dollars towards their oral health needs, including treatments that restore function to the mouth. Dentists often provide detailed cost breakdowns and payment plans to help patients budget for their implant journey:
- Review insurance benefits for prosthodontic coverage
- Explore in-house financing options
- Consider dental savings plans or HSAs
- Discuss payment plans with the dental office
- Investigate third-party healthcare financing
Comparison of Long-Term Costs With Other Dental Solutions
Dental implants offer long-term cost-effectiveness compared to other tooth replacement options. While the initial investment may be higher, implants can last a lifetime with proper care, reducing the need for frequent replacements or adjustments. Traditional bridges and dentures typically require replacement every 5-10 years, incurring additional costs over time.
The Harmony Dental Group provides patients with a comprehensive cost analysis to illustrate the long-term value of dental implants. This comparison takes into account factors such as durability, maintenance requirements, and impact on oral health:
Maintenance and Longevity of Dental Implants
Dental implants require proper care to ensure their longevity and function. This section covers best practices for implant maintenance, emphasizing the importance of regular dental check-ups. It also addresses common issues patients may encounter and provides practical solutions, helping to maximize the lifespan of dental implants and maintain overall oral health.
Best Practices for Caring for Dental Implants
Proper care for dental implants involves diligent oral hygiene practices. Patients should brush twice daily with a soft-bristled toothbrush and use non-abrasive toothpaste to protect the implant surface. Flossing around the implant is crucial to remove plaque and prevent peri-implantitis, a condition that can lead to implant failure.
The Harmony Dental Group recommends using interdental brushes or water flossers to clean hard-to-reach areas around implants. Regular dental check-ups and professional cleanings are essential for maintaining implant health and detecting any potential issues early. Patients should avoid smoking and limit consumption of staining substances to preserve the appearance of their implant-supported crowns.
Regular Dental Check-Ups and Their Importance
Regular dental check-ups are crucial for maintaining the longevity of dental implants. The Harmony Dental Group recommends biannual visits to monitor implant health, assess surrounding tissue, and perform professional cleanings. These appointments allow dentists to detect early signs of complications, such as peri-implantitis or loosening of the implant, ensuring prompt intervention.
During check-ups, dentists evaluate the stability of the implant and the condition of the prosthetic crown. They may take X-rays to examine bone levels and check for any signs of infection or bone loss. Patients should communicate any discomfort or changes they've noticed, as early detection of issues can significantly improve treatment outcomes:
Common Issues and Their Solutions
Patients may experience common issues with dental implants, such as peri-implantitis, a condition characterized by inflammation of the surrounding tissues. The Harmony Dental Group advises early intervention through professional cleaning and antimicrobial treatments to prevent progression. In cases of implant loosening, dentists may recommend bone grafting or implant replacement to restore stability.
Fractures in implant-supported crowns can occur due to excessive force or wear. Dentists at The Harmony Dental Group address this by evaluating the patient's bite and replacing the damaged crown with a more durable material. For patients experiencing discomfort or sensitivity around their implants, a thorough examination is conducted to identify and treat the underlying cause, ensuring long-term implant success.
Frequently Asked Questions
What are dental implants and how do they restore smiles?
Dental implants are artificial tooth roots surgically placed into the jawbone to support replacement teeth. They provide a permanent solution for missing teeth, restoring natural-looking smiles and oral function. Made of biocompatible materials, implants fuse with bone, offering stability and longevity for a confident, healthy smile.
How long does the dental implant procedure typically take?
The dental implant procedure typically takes 3-6 months from start to finish. This includes initial consultation, placement of the implant, healing period, and attachment of the crown. However, the actual surgical procedure for placing the implant usually takes around 1 hour per tooth.
Are there different types of dental implants available?
Yes, there are different types of dental implants available. The Harmony Dental Group in Norwalk, CT offers various options, including endosteal implants (placed in the jawbone) and All-on implants for full-arch restoration. Each type is tailored to meet specific patient needs and oral health conditions.
Who qualifies as a good candidate for dental implants?
Good candidates for dental implants are adults with healthy gums, sufficient bone density, and overall good health. They should be non-smokers or willing to quit, committed to oral hygiene, and free from conditions that could impair healing. Regular dental visits are essential for long-term success.
How should dental implants be maintained for long-lasting results?
Regular brushing, flossing, and dental check-ups are essential for maintaining dental implants. Patients should avoid smoking and chewing hard foods. Using a soft-bristled toothbrush and non-abrasive toothpaste helps prevent damage. Professional cleanings every six months ensure long-lasting results and optimal oral health. Water picks are highly recommended.
Conclusion
Dental implants offer a durable, long-lasting solution for replacing missing teeth, restoring both function and appearance while preserving oral health. The Harmony Dental Group provides comprehensive care, from initial consultation to post-surgery maintenance, ensuring patients receive personalized treatment tailored to their unique needs. By understanding the types of implants available, the surgical process, and factors influencing candidacy, patients can make informed decisions about their dental restoration journey. Regular check-ups and proper maintenance are crucial for maximizing the longevity of dental implants, allowing patients to enjoy the benefits of a restored smile for years to come.